Parasite triggered painful uvula ulcer in man 5 years after he caught it in South America
A man unwittingly picked up a parasite, and years later, it triggered a throat infection.
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
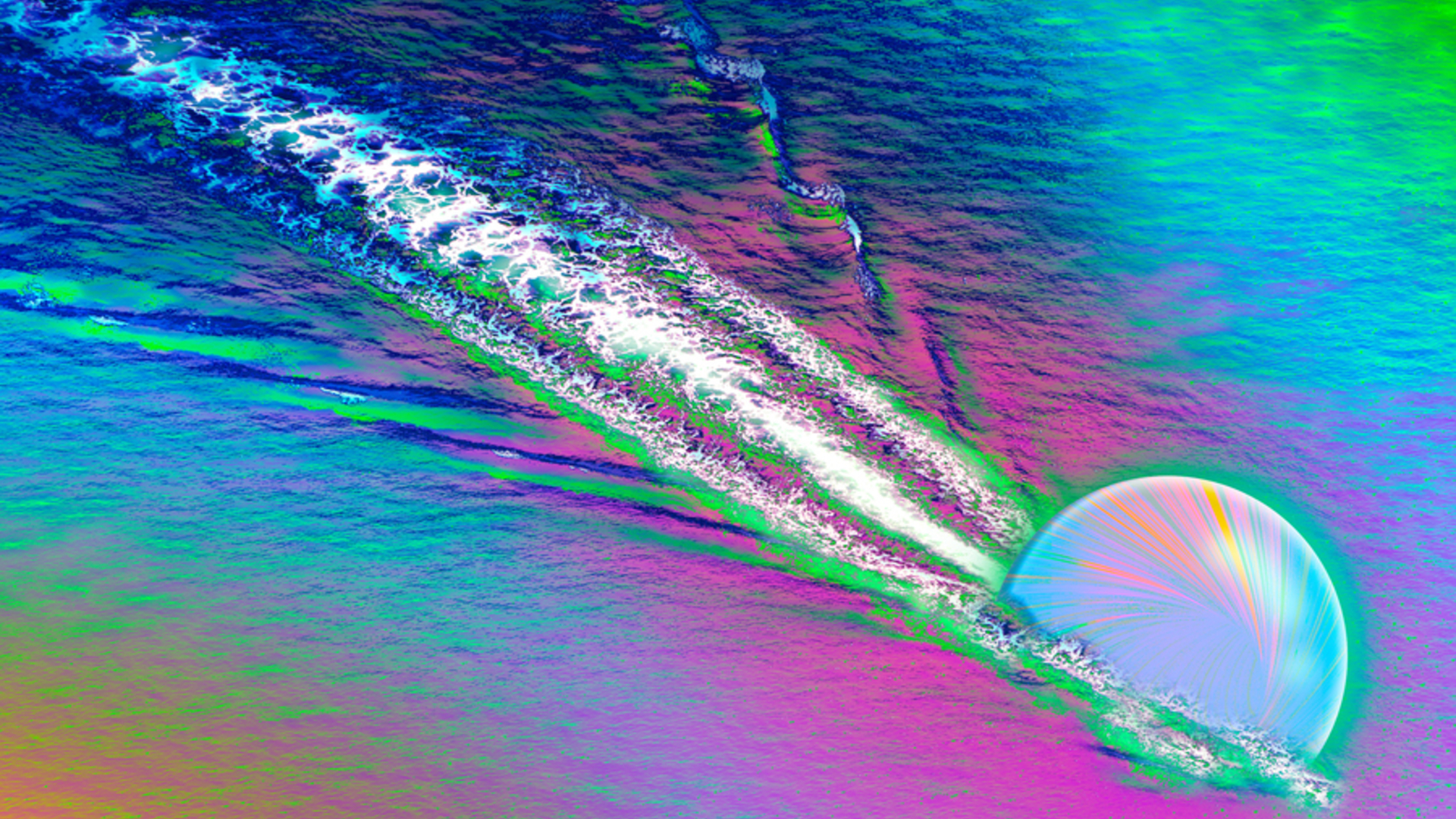
A large, snow-white ulcer swelled up on the dangly tissue at the back of a man's throat, but doctors couldn't immediately explain why. It turns out that a single-celled parasite was the culprit, and it had likely been hanging around the man's body for five years.
According to a new report of the case, published Thursday (Aug. 17) in the journal JAMA Otolaryngology–Head & Neck Surgery, the 62-year-old man initially went to the doctor about a sore throat. He had no recent travel history or contact with sick people, but the midline of his throat had been hurting for two weeks. An examination of his throat revealed bumps decorating the tissue, as well as sticky, yellow mucus and an ulcer on his uvula, the tissue that hangs in the back of the mouth.
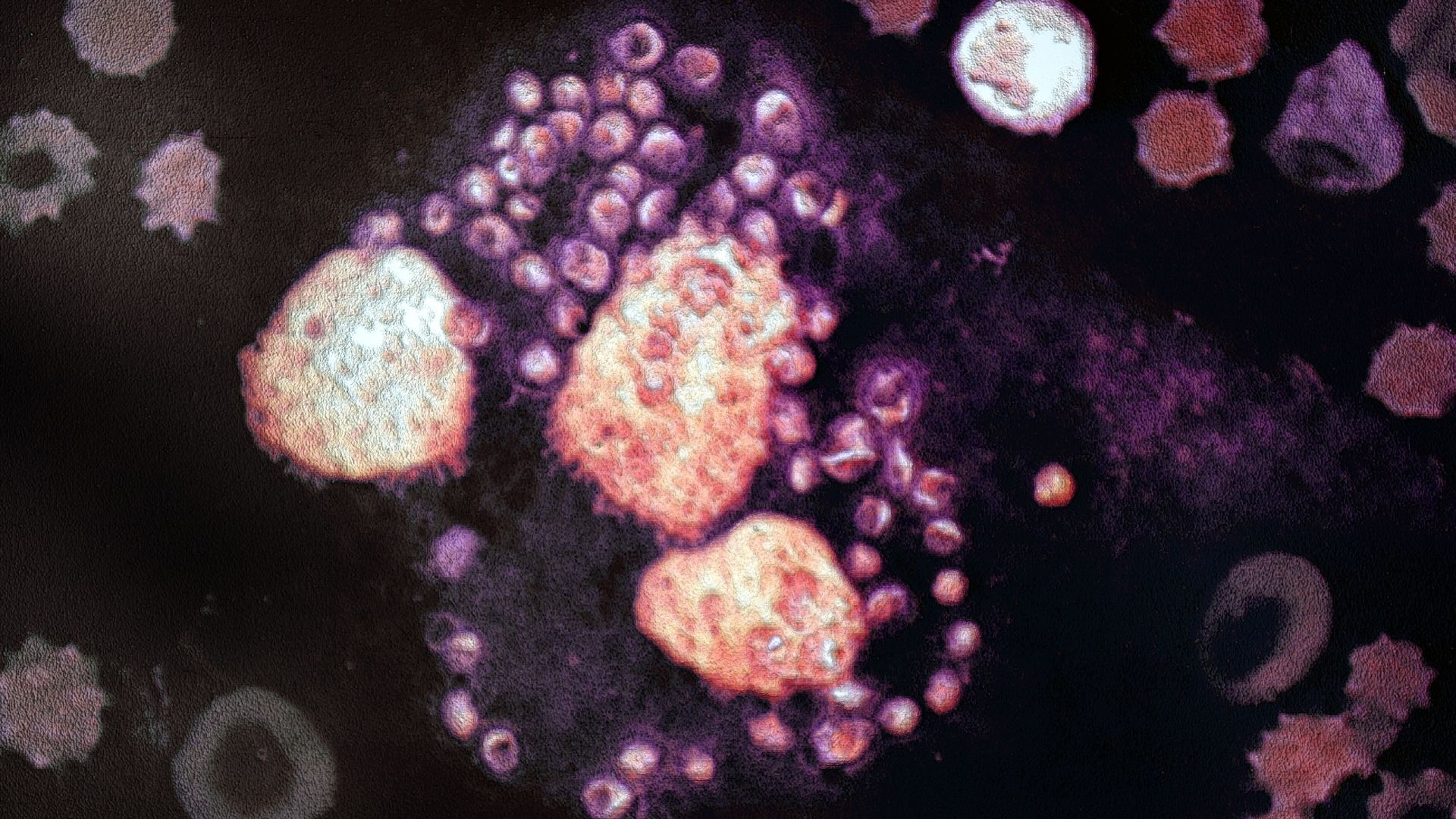
An initial round of antibiotic and antifungal treatment didn't work, and the man's symptoms worsened over the following two weeks. Searching for the infection's cause, the doctors tested the patient for COVID-19; the viral disease mononucleosis, or "mono"; and group A Streptococcus, the bacteria behind strep throat. All of the tests came back negative. Then, they took a tissue sample from the man's throat. The sample was teeming with immune cells that usually help fight infections.
However, the cause of the infection remained elusive. To no avail, the doctors prescribed antibiotics, antifungals, heartburn medications and steroids that didn't relieve the man's symptoms.
Related: Cambrian fossils show oldest example of parasites in action
In the end, a deep dive into the man's medical history and closer examination of his ulcer biopsy would reveal the cause of his illness.
Five years prior, he'd traveled to Guyana, in South America, and subsequently sought medical treatment for multiple small lumps that had grown beneath the skin of his neck. At the same time, he also had a larger, 1.6-inch (4 centimeters) bump that indicated a deep infection of the skin. At that time, the man tested negative for disease-causing fungi and bacteria, and after antibiotics failed to treat the bumps, doctors surgically removed the largest nodules. The smaller ones resolved on their own.
Get the world’s most fascinating discoveries delivered straight to your inbox.
However, years down the line, the mysterious ulcer appeared on the man's uvula, and doctors uncovered both its cause and the likely cause of the previous lumps: Leishmania braziliensis, a species of single-celled parasite that causes an infection called leishmaniasis.
Humans can contract L. braziliensis through the bites of infected sand flies, according to the Centers for Disease Control and Prevention (CDC). The parasites live in the tropics, subtropics and Southern Europe, and the CDC advises travelers to take measures to avoid sand fly bites while visiting affected locations.
The most common form of leishmaniasis, cutaneous leishmaniasis, causes skin sores that typically appear weeks or months after the initial fly bite or, more rarely, years later. The sores are often painless and usually heal on their own, but they can persist for months to years and leave scars. And with some Leishmania species, there's also a risk the parasite will spread elsewhere if left untreated in the skin.
In the man's case, he initially had cutaneous leishmaniasis, which caused the bumps on his neck. The infection then spread from his skin to the mucous membranes of his mouth and throat, causing what's known as mucosal leishmaniasis. The disease causes symptoms years to decades after a person's original cutaneous bumps, and when it occurs, it's typically if those first bumps went untreated or were treated ineffectively, the CDC notes.
The man's doctors analyzed a sample of his original skin bumps, collected five years earlier, and a stain revealed the parasites nestled inside his skin cells.
To finally kill the parasites, the doctors prescribed a month-long course of the leishmaniasis drug miltefosine. This treatment "led to complete resolution of the mucosal lesion and associated symptoms," the case report authors concluded.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.
 Live Science Plus
Live Science Plus