Boy Gets Food Allergies from Blood Transfusion
A boy in Canada mysteriously became allergic to fish and nuts after he received a blood transfusion, according to a new case report.
A boy in Canada mysteriously became allergic to fish and nuts after he received a blood transfusion, according to a new case report.
The 8-year-old boy had no history of being allergic to any foods, and was undergoing treatment for medulloblastoma, a type of brain cancer. A few weeks after receiving a blood transfusion, he experienced a severe allergic reaction called anaphylaxis within 10 minutes of eating salmon, according to the report, published online today (April 7) in the Canadian Medical Association Journal.
His doctors suspected that the blood transfusion had triggered the reaction, they wrote in the report. After treating the patient with a drug containing antihistamines, the doctors advised him to avoid fish and to carry an epinephrine injector in case he had another reaction.
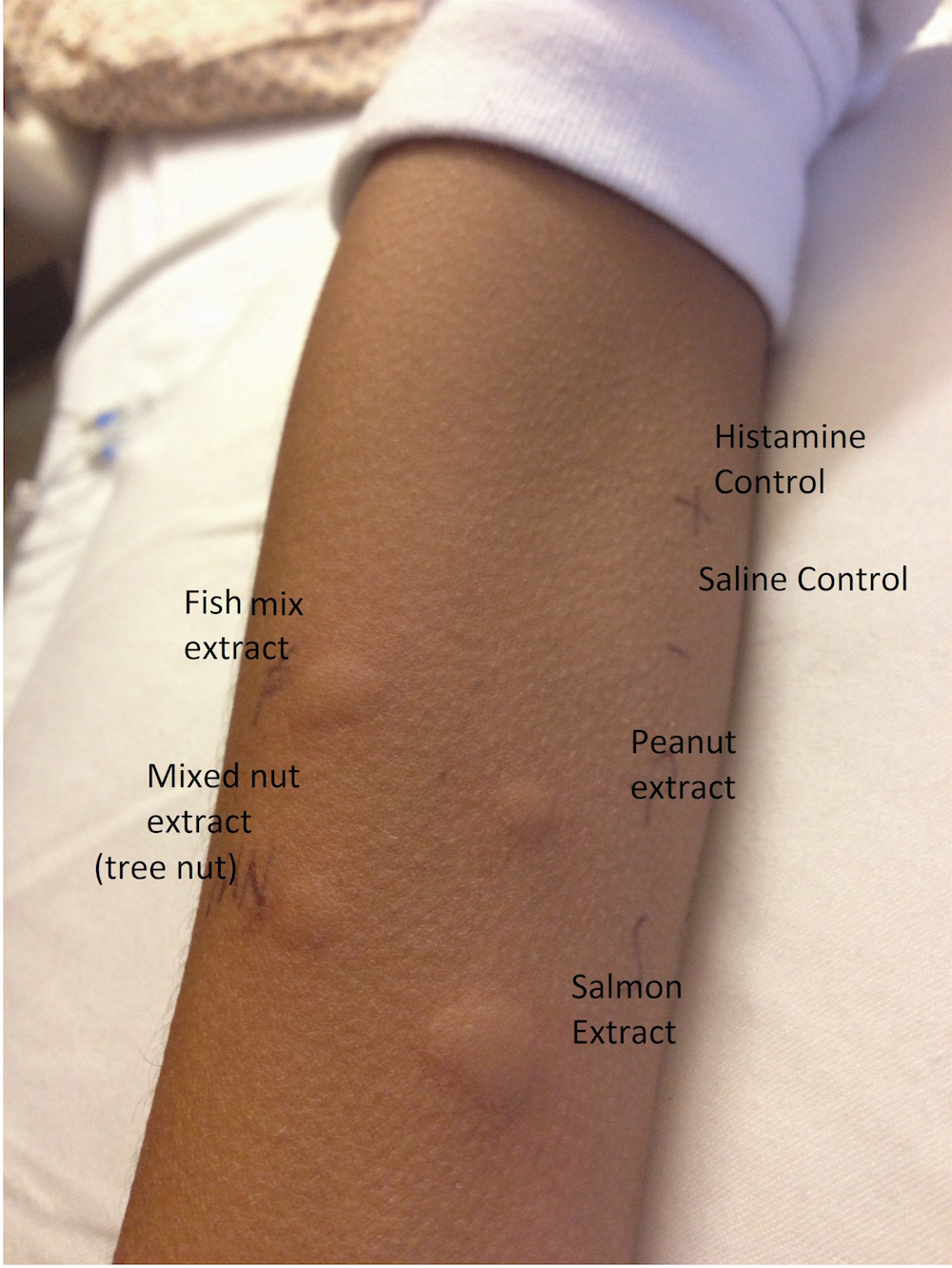
But four days later, the boy was back in the emergency department after eating a chocolate peanut butter cup. Blood tests and a skin prick test suggested that he was allergic — at least temporarily — to peanuts and salmon, so his doctors advised him to avoid nuts and fish.
"It's very rare to have an allergic reaction to a previously tolerated food," said the report's senior author, Dr. Julia Upton, a specialist in clinical immunology and allergy at the Hospital for Sick Children in Toronto. "The overall idea is that he wasn't allergic to these foods," but in the blood transfusion, he received the protein that triggers an allergic reaction to them, she said.
That protein, called immunoglobulin E, is an antibody associated with food allergies, Upton said. When it encounters a specific allergen, it causes immune cells to release chemicals such as histamine that lead to an allergic reaction.
However, because the boy's body itself did not make such antibodies against fish and nuts, his doctors said they suspected his allergies would go away within a few months.
Get the world’s most fascinating discoveries delivered straight to your inbox.
Acquiring allergies from a blood donor is rare, but not without precedent. The researchers found two other case reports, both in adults, in which patients acquired temporary allergies from blood plasma. In a 2007 case, an 80-year-old woman had an anaphylactic reaction to peanuts. An investigation showed that her 19-year-old plasma donor had a peanut allergy, according to the report in the journal Archives of Internal Medicine.
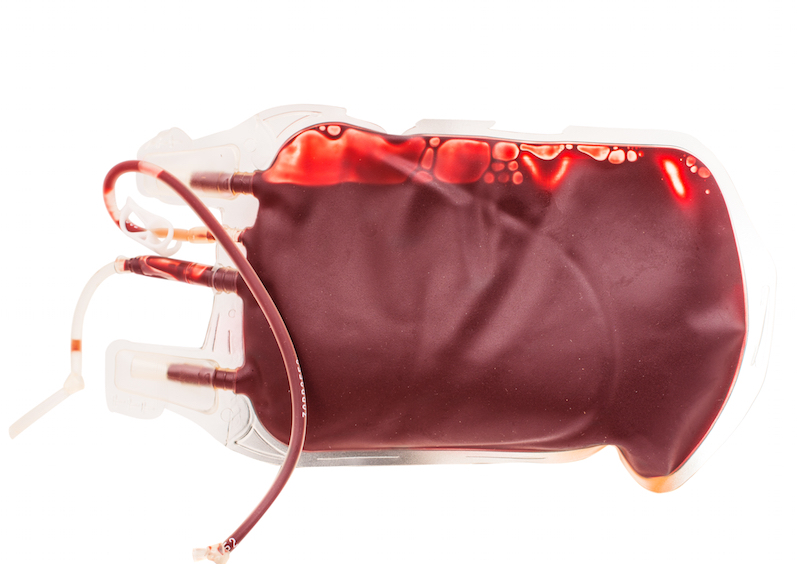
In the new case, the 8-year-old also received plasma, the liquid part of blood that contains antibodies. The researchers inquired about the donor to Canadian Blood Services, and found that the donor did have an allergy to nuts, fish and shellfish. The service did not have any more blood from the donor, and subsequently excluded the individual from making future donations, the researchers said.
About five months later, blood tests showed that the boy's immunoglobulin E levels to salmon and peanut were undetectable. By six months, his parents had gradually and successfully reintroduced nuts and fish back into their son's diet.
However, Upton said, "In general, we would recommend that this be done under medical supervision," just in case there is a medical emergency.
It's unclear how doctors could prevent future cases, she said. Neither Canadian nor American blood service organizations bar people with allergies from donating blood. And testing donated blood for levels of immunoglobulin E doesn't always predict allergies. Some people with high levels of immunoglobulin E don't have allergies, and others with low levels of the protein do, she said.
"Clearly, the safety of the [blood] supply is of everyone's utmost concern," but more research is needed to determine how best to avoid the transfer of allergies, and how frequently this happens, Upton said.
"I think it's hard to make sweeping recommendations based on one case report," Upton said.
In the United States, "If a donor is feeling well and healthy on the day of donation, they are typically eligible to donate," said Dr. Courtney Hopkins, the acting chief medical officer for the east division of the American Red Cross. "We will defer donors on the day of donation if they are not feeling well and healthy, if they have a fever, or if we notice they have problems breathing through their mouth."
Donors can learn more about blood-donation eligibility here. Individuals with allergies shouldn't be dissuaded from donating, Hopkins added.
"We always need blood. We always need blood donors," Hopkins told Live Science.
Follow Laura Geggel on Twitter @LauraGeggel. Follow Live Science @livescience, Facebook & Google+. Original article on Live Science.

Laura is the managing editor at Live Science. She also runs the archaeology section and the Life's Little Mysteries series. Her work has appeared in The New York Times, Scholastic, Popular Science and Spectrum, a site on autism research. She has won multiple awards from the Society of Professional Journalists and the Washington Newspaper Publishers Association for her reporting at a weekly newspaper near Seattle. Laura holds a bachelor's degree in English literature and psychology from Washington University in St. Louis and a master's degree in science writing from NYU.
 Live Science Plus
Live Science Plus