Possible cause of COVID-19 blood clots found
COVID-19 appears to spur the production of special antibodies known to trigger blood clots.
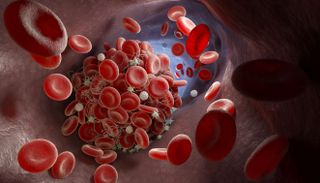
One of the many dangers of COVID-19 is the disease's mysterious ability to promote blood clots throughout the body. Now, a new study may explain why — the disease appears to spur the production of special antibodies known to trigger blood clots.
These so-called "autoimmune antibodies" or "autoantibodies" attack a person's own tissues. Specific types of autoantibodies called "antiphospholipid autoantibodies" attack cells in such a way as to promote blood clots.
In the study, published Nov. 2 in the journal Science Translational Medicine, researchers detected these autoantibodies in about half of patients hospitalized with COVID-19.
Related: Coronavirus Live Updates
Prior to the COVID-19 pandemic, these autoantibodies were typically seen in people who have an autoimmune disorder known as antiphospholipid syndrome, or APS. This syndrome affects about 1 in every 2,000 people, and it triggers dangerous blood clots inpatients' arteries and veins.
"Now, we're learning that autoantibodies could be a culprit" in complications of COVID-19, study co-author Dr. Yogen Kanthi, an assistant professor at the Michigan Medicine Frankel Cardiovascular Center, said in a statement. They may play a role in a vicious cycle of blood clotting and inflammation that "makes people [with COVID-19] who were already struggling even sicker," Kanthi said.
Clot-causing antibodies
In the new study, the researchers analyzed blood samples from 172 patients hospitalized with COVID-19. Overall, 52% of these patients had antiphospholipid autoantibodies in their blood.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
What's more, when the researchers injected these autoantibodies into mice used to study blood clots in a lab, they observed "a striking amount of clotting in animals — some of the worst clotting we've ever seen," Kanthi said.
In both COVID-19 and APS, it's unclear why the body produces these clot-causing antibodies. With APS, scientists think that the disease is caused by a combination of a person's genetics and environmental exposures — including exposures to certain viruses, according to the National Institutes of Health.
The researchers also found a link between levels of autoantibodies and levels of another substance in the blood called neutrophil extracellular traps (NETS). These are web-like structures released by white blood cells (known as neutrophils) that can trap viruses and other pathogens. The authors hypothesize that autoantibodies and NETS may act together to promote blood clots.
However, more research is needed to better understand the role of these autoantibodies in COVID-19, and what's triggering their production.
Severe cases of COVID-19 are now commonly treated with anti-clotting drugs to reduce the risk of life-threatening blood clots. But it's possible that inhibiting or removing the autoantibodies could also improve patients' outcomes, the authors said.
If that's the case, patients might benefit from a treatment called plasmapheresis, which is sometimes used in cases of severe autoimmune disease and involves removing, filtering and returning plasma, the liquid portion of blood that contains the harmful antibodies.
The study also raises questions about the use of convalescent plasma, or plasma from recovered COVID-19 patients, to treat the disease, since that plasma may contain these harmful autoantibodies in addition to helpful antibodies against COVID-19. Future studies are needed to investigate this concern, and the authors are currently conducting research to see how long the autoantibodies stick around after people recover from COVID-19.
Originally published on Live Science.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
